– Report also provides latest statistics and information on Alzheimer’s prevalence, incidence, mortality and cost of care in North Carolina and nationally –
The Alzheimer’s Association 2024 Alzheimer’s Disease Facts and Figures report reveals that both dementia caregivers and health care workers report difficulties in navigating dementia care within the U.S. health care system. The report provides an in-depth look at the latest national and state-level statistics on Alzheimer’s disease prevalence, mortality, caregiving, dementia care workforce and costs of care. The new report estimates that 6.9 million people age 65 and older in the U.S. are living with Alzheimer’s dementia, including 210,500 in North Carolina.
This year the cost of caring for people living with Alzheimer’s and other dementias is projected to reach $360 billion — a $15 billion increase from a year ago. This does not include unpaid care provided by family caregivers and friends. Last year in North Carolina there were 373,000 dementia family caregivers, providing 723 million hours of unpaid care valued at $10.9 billion.
“The new Facts and Figures report sheds light on the continued pressures that many North Carolina families are going through as a result of Alzheimer’s and other dementias. As the number of individuals living with Alzheimer’s continues to grow, ensuring patients, their caregivers and families have a clear understanding of how to navigate dementia care resources is critical to improving health outcomes.”
Katherine L. Lambert, Alzheimer’s Association Regional Leader for NC, SC & GA
Here are the biggest takeaways from this year’s report for North Carolina:
More Americans have Alzheimer’s disease.
- An estimated 6.9 million Americans aged 65 and older have Alzheimer’s dementia, including more than 210,000 in North Carolina.
- It is estimated that approximately 200,000 Americans under the age of 65 have younger-onset Alzheimer’s.
Deaths due to Alzheimer’s disease are increasing.
- Between 2000 and 2021, the number of deaths from Alzheimer’s disease in the U.S. as recorded on death certificates more than doubled, increasing 141%, while deaths from the number-one cause of death in the U.S. (heart disease) decreased 2.1%.
- Alzheimer’s disease was the fifth-leading cause of death among individuals age 65 and older in 2021 (the most recent year for mortality data).
- In North Carolina, deaths due to Alzheimer’s have increased an alarming 147% between 2000 and 2021. There were 4,260 deaths in the state from Alzheimer’s disease in 2021.
Alzheimer’s is one of the most costly diseases for individuals, families, caregivers, and the government.
- The total cost for caring for people with Alzheimer’s and other dementias in the United States is projected to reach $360 billion in 2024. In addition, family and friends provided nearly $350 billion ($346.5) in unpaid caregiving in 2023.
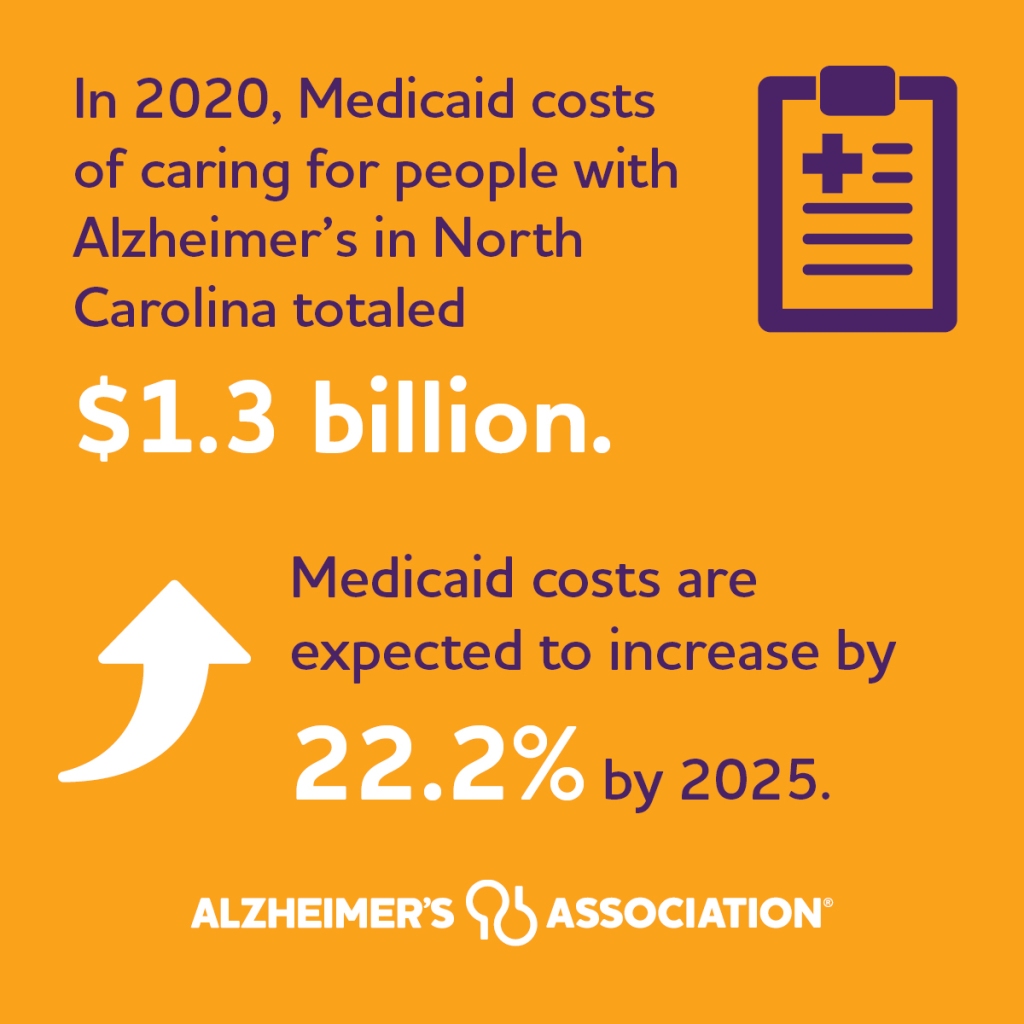
- In North Carolina the Medicaid costs of caring for people with Alzheimer’s are estimated at $1.3 billion. Between 2020 to 2025, these costs are projected to increase by 22%.
- In 2023, the per capita Medicare spending in North Carolina on people with dementia was $27,591 for each person.
- Without new treatments and advancements in care, the total cost for caring for people living with Alzheimer’s and other dementias is projected to reach nearly $1 trillion in 2050.
Caregiving time, costs of care continue to rise.
- In 2023, 11.475 million caregivers provided nearly 18.4 billion hours of unpaid care, a contribution to the nation valued at $346.6 billion.
- In North Carolina, 373,000 caregivers provided a total of 723 million hours of unpaid care, valued at a total of $10.9 billion.
- The total lifetime cost of care for someone with dementia is estimated at almost $400,000 ($394,683) with 70% of these costs borne by family caregivers in the forms of unpaid caregiving and out-of-pocket expenses.
- Sixty percent of caregivers of people with Alzheimer’s or another dementia were employed in the past year. However, many of these caregivers had to make major changes to their work schedules because of caregiving responsibilities: 57% said they had to go in late, leave early or take time off and 16% had to take a leave of absence.
A shortage of dementia care specialists and direct care workers compromises care for people living with dementia.
- 55% of PCPs caring for people living with Alzheimer’s report there are not enough dementia care specialists in their communities.
- In 2021, there were only 158 geriatricians in North Carolina. By 2050, 535 geriatricians will be needed to care for residents across the state living with Alzheimer’s dementia.
- Twenty U.S. states have been termed “dementia neurology deserts,” meaning they are projected to have fewer than 10 neurologists per 10,000 people with dementia in 2025. (States include: AL, AR, DE, HI, IA, ID, KS, KY, ME, MS, MT, ND, NM, NV, OK, SC, SD, VT, WV, WY)
- Between 2012 and 2022, the number of direct care workers increased from 3.2 million to 4.8 million due to growing demand for long-term care. More than 1 million additional direct care workers are needed to meet future care demands between 2021 and 2031 — more new workers than in any other single occupation in the United States.
- Twenty-one states expect to see a 30% to 40% increase in the size of this workforce, while two states — Arizona and Nevada — are expected to increase by more than 50%.
- Although sizable, these employment projections fall short of true workforce demand.
- In 2020, there were an estimated 65,150 home health and personal care aids in North Carolina. By 2030, 82,070 will be needed — a 26% increase.
Special Report Finds Difficulties in Navigating Dementia Care within the U.S. Health Care System
An accompanying special report, “Mapping a Better Future for Dementia Care Navigation,” provides a comprehensive look into dementia care navigation by surveying dementia caregivers and health care workers on their experiences, challenges, awareness and perceptions of care navigation in dementia care. Dementia care navigation provides clinical and nonclinical support to people living with dementia and their caregivers to overcome barriers that compromise care and health outcomes.
Key findings:
- In 2023, 11.5 million family and other caregivers of people living with Alzheimer’s or other dementias provided an estimated 18.4 billion hours of unpaid help. On average, this represents nearly 31 hours of care per caregiver per week or 1,612 hours per caregiver per year.
- A majority of caregivers (70%) report that coordination of care is stressful.
- More than half of the caregivers surveyed (53%) said that navigating health care was difficult.
- 2 in 3 caregivers (66%) also have difficulty finding resources and support for their needs.
- The top five stressors for caregivers are:
- Cost (reported by 42% of caregivers).
- Coordinating with multiple doctors (36%).
- Securing appointments (35%)
- Getting help taking a break (35%).
- Finding appropriate doctors (32%).
- Care navigation facilitates medical and social support to alleviate patient and caregiver stress. Despite coordinating care and scheduling being top stressors for caregivers, only half of the caregivers surveyed (51%) have ever talked with a health care professional about challenges finding their way through the health care system or asked for help with dementia care.
- Black and Hispanic caregivers report managing care on a daily basis (43% and 45%, respectively) compared to White caregivers (31%).
- The vast majority of dementia caregivers (97%) say that they would find navigation services helpful. Services cited most often by caregivers include:
- A 24/7 helpline (36%).
- Help with coordinating care and communication between different specialists (34%).
- Getting help in understanding their care recipient’s condition (34%).
- 60% of health care workers surveyed believe that the U.S. health care system is not effectively helping patients and their families navigate dementia care. Nearly half (46%) say that their organizations do not have a clearly defined process for care coordination and clinical pathways for patients with mild cognitive impairment (MCI), Alzheimer’s disease or other dementia.
“The big takeaway from this year’s special report is that dementia caregivers want and need help navigating the complex health care system and accessing community-based services. Given the added complexities of dementia care, we hope our report will encourage health systems and practices to think more intentionally about the challenges facing dementia caregivers and formalize dementia care navigation programs to help them.”
Katherine L. Lambert, Alzheimer’s Association Regional Leader for NC, SC & GA


Full text of the Alzheimer’s Association 2024 Alzheimer’s Disease Facts and Figures report, including the accompanying special report, “Mapping a Better Future for Dementia Care Navigation,” can be viewed at alz.org/facts.
About 2024 Alzheimer’s Disease Facts and Figures:
The Alzheimer’s Association 2024 Alzheimer’s Disease Facts and Figures report is a comprehensive compilation of national statistics and information on Alzheimer’s disease and related dementias. The report conveys the impact of Alzheimer’s on individuals, families, government and the nation’s health care system. Since its 2007 inaugural release, the report has become the preeminent source covering the broad spectrum of Alzheimer’s issues. The Facts and Figures report is an official publication of the Alzheimer’s Association.